
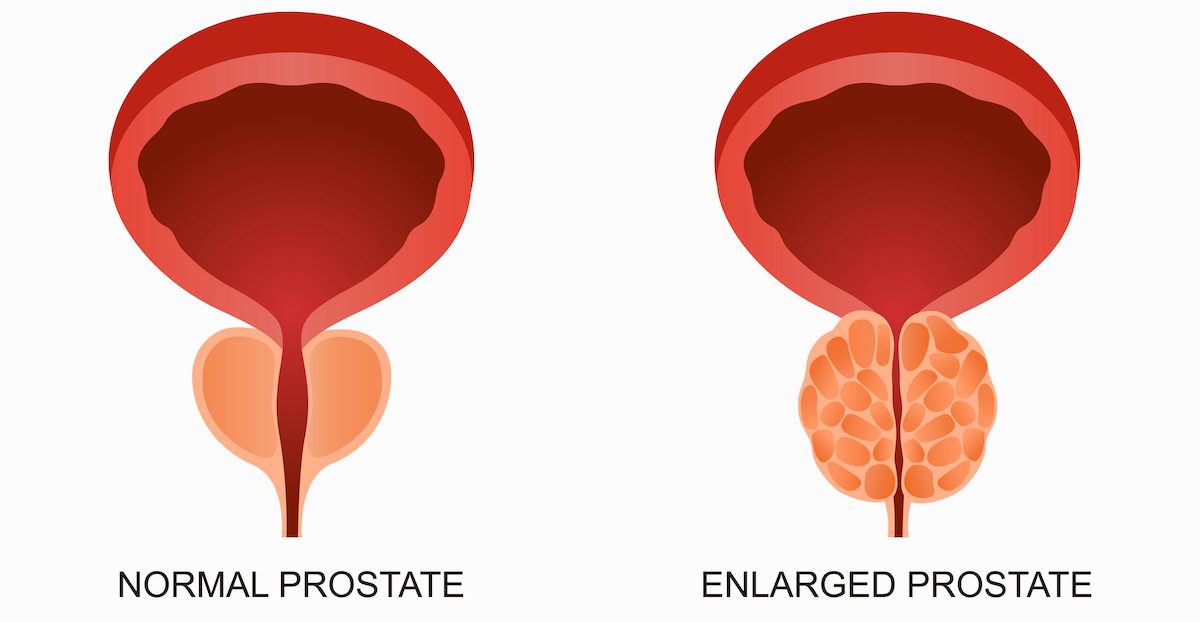
Benign Prostatic Hyperplasia (BPH) is a common, non-cancerous enlargement of the prostate gland that occurs in many men as they age. As the prostate grows, it can narrow or block the urethra—the channel that carries urine out of the body—resulting in bothersome urinary symptoms.
Although BPH does not increase the risk of prostate cancer, it can significantly impact comfort, sleep, and quality of life. The good news: BPH is very treatable, and modern therapies offer excellent long-term outcomes.
Symptoms of BPH
BPH symptoms result from the obstruction of urine flow and can range from mild to severe. Common symptoms include:
- Frequent urination, especially at night (nocturia)
- Difficulty starting urination (hesitancy)
- Weak or interrupted urine stream
- Incomplete emptying of the bladder
- Urgency and possible leakage
Over time, untreated BPH can lead to complications such as bladder stones, blood in the urine, inability to urinate, urinary tract infections, or kidney damage.
Causes and Risk Factors
The exact cause of BPH isn’t fully understood, but it is linked to hormonal changes associated with aging—particularly the balance between testosterone and estrogen. Risk factors include:
- Age (especially over 50)
- Family history of BPH
Diagnosis
Diagnosis typically begins with a review of symptoms and medical history. Common diagnostic tools include:
- Digital rectal exam (DRE) to assess prostate size
- Urinalysis to rule out infection or blood in the urine
- Prostate-specific antigen (PSA) blood test
- Prostate ultrasound or MRI
- Uroflowmetry and post-void residual measurement
- Cystoscopy to view the inside of the prostate and bladder with a video camera
Treatment Options
Treatment for BPH depends on the severity of symptoms and the degree of urinary obstruction.
Lifestyle Modifications:
- Reduce caffeine, tea and alcohol, which can irritate the bladder and increase urgency.
- Avoid drinking fluids 2–3 hours before bedtime to reduce nighttime urination.
- Practice timed voiding, such as going to the bathroom every 2–3 hours during the day.
- Use “double voiding”—urinate, wait 20–30 seconds, and try to urinate again—to help fully empty the bladder.
- Manage constipation with adequate fiber and hydration, as a full rectum can worsen urinary symptoms.
Medications:
- Alpha-blockers: Relax prostate and bladder neck muscles to ease urination
- 5-alpha-reductase inhibitors: Shrink the prostate by blocking hormonal changes
- Combination therapy: Uses both medications for enhanced effect
Surgical Options:
Aquablation®
A robot-assisted, ultrasound-guided therapy that uses a high-velocity waterjet to precisely remove prostate tissue.
- Minimally invasive with reduced heat-related side effects
- May preserve ejaculatory function in select patients
- May be limited by large prostate size.
- Typically performed under general anesthesia
- Less durable than HoLEP
HoLEP (Holmium Laser Enucleation of the Prostate)
A state-of-the-art laser procedure that removes obstructing tissue regardless of prostate size.
- Highly durable
- Low retreatment rate (<1–2%)
- Suitable for very large prostates
- Ideal for patients in urinary retention or on blood thinners
As a fellowship-trained HoLEP specialist at UCI, I offer this procedure for men seeking long-term, definitive relief.
Ongoing Management
Men with BPH benefit from regular follow-up to monitor symptoms and assess whether treatment adjustments are needed. With proper care, most men can manage BPH effectively and maintain good urinary function.
